By James Grant, ATC
IMU Step’s new metric, Impact Asymmetry, represents a major step forward in the ability to track a patient or athlete’s lower limb loading pattern across and within sessions. This collection method opens up the door to a whole new range of tracking insights, as well as some novel approaches that you should start thinking about.
I will take you through the three most important next steps you can take with the metric and dive a bit deeper into why these are important to your athletes or patients. While my formal background is in athletic training, I have spent most of my professional career in the wearable tech space, so I will be exploring the metric from both a rehabilitation and general load monitoring standpoint. This brings me to use number 1
1. Identify at-risk loading patterns
IMU Step’s Impact Asymmetry measure makes it much easier to build normative values for a specific patient or population. When you first get started with tracking lower limb asymmetry, the easiest place to start is to use 0% asymmetry as the idealized norm for each new subject. Prescribe an inherently symmetrical activity, such as running on a treadmill, and compare the asymmetry of your subject to the idealized norm. If the subject’s asymmetry is above a certain threshold, 5% asymmetrical for example, you may want to investigate their injury history and current status to determine what may be causing the asymmetry.
We know that in the real world, most people are not perfectly symmetrical. Most people have some amount of functional asymmetry that doesn’t necessarily lead to a dysfunction or pain. That is why the gold standard is a baseline of the patient against themselves, rather than a group. In that scenario, assuming we stick to the 5% threshold, I would flag a 5% deviation from their average not a 5% deviation from symmetrical. This would then give me an at-risk designation customized for my specific patients.

This patient is presenting with a 25% asymmetry and would definitely warrant further intervention
2. Track recovery across time
Tracking Impact Asymmetry longitudinally is a great way to measure rehab progress over time. With a lower limb injury, a patient will usually present with a large discrepancy in early rehab that regresses back towards symmetry over time. If we have a baseline for our patient, we know exactly what functional asymmetry value we want to achieve by the end of rehab; if we don’t have a baseline, we can use 0% asymmetry as a rough value. Over the course of my rehab protocol, I can then check the patients objective progress against planned benchmarks and adjust my rehab accordingly to accommodate each specific patient.
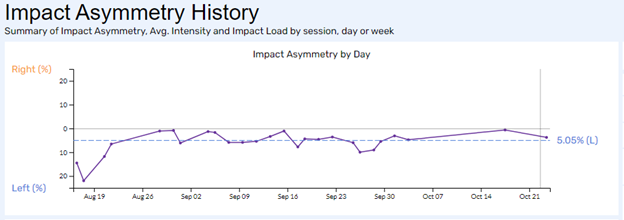
This is the recovery timeline of a lisfranc fracture recovery. You can clearly see her progress over time as she gains symmetry
3. Build rehab protocols
Impact Asymmetry is a useful metric to proactively plan your sessions from a “load quality” standpoint. Combined with Impact Load, which communicates “load volume” you can create a solid idea of what stresses and loads your patient will experience for each exercise you prescribe. To get to this point, you must be diligent about taking good footnotes so that you can build accurate data into your drill library. The payoff is certainly worth the effort once you get to a point where you can precisely plan every step in your rehab and avoid drills or exercise that put unnecessary strain on your patient.
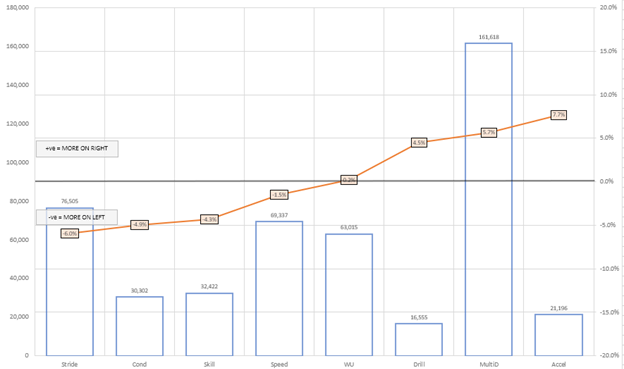
If I were trying to build a symmetrical loading protocol for this patient, I would avoid Stride and Accel exercises
Explore more asymmetry resources:
Practical Examples of Using IMU-Step to Modify Outcomes: Asymmetry and Impact Load in the Real World – An IMU webinar with Andrew Gray
What is Impact Asymmetry – A breakdown of how the metric is calculated and what it measures
Please feel free to reach out to us with any questions and we will be happy to share best practices and help you as you prepare for monitoring asymmetry.


